They are called biopolymeric patches. The name sounds complicated, but the function is simple and revolutionary for those who have suffered a myocardial infarction whose current treatment is merely palliative care or, in more severe cases, heart transplantation. Developed at CICECO, University of Aveiro (UA), in collaboration with scientists from the University of Helsinki, these materials made from natural resources may be the solution to repair heart tissue affected by infarction.
Made from two protein materials, gelatin and lysozyme nanofibrils (a protein found, for example, in chicken eggs), these biopolymeric patches were developed through electro-spinning, a technique that allows the production of fibers. Through this procedure, the team of researchers from UA managed to obtain extremely long and thin fibers made of gelatin and protein nanofibrils that are deposited on top of each other, forming a fibrous patch.
All over the world, fibrous gelatin patches have been produced before, but their properties and functionality fell short of what is needed to help regenerate myocardial tissues from a heart that has suffered a heart attack. The addition of these protein nanofibrils constitutes an innovative strategy that allowed the improvement of several properties and functionalities of the patch such as mechanical performance, antioxidant activity and its bioresorbability .
"The addition of the lysozyme nanofibrils resulted in an increase in the mechanical performance of the patches, an important factor considering the place where the patch will be implanted, the heart," explains Tiago Carvalho, Doctoral student at CICECO-Aveiro Institute of Materials, one of UA's research units.
The study published in the Advanced Functional Materials journal, points out other advantages to the newly developed patches: specifically, a considerable increase in antioxidant activity, also extremely important, since damaged tissue, such as myocardium after a heart attack, contains compounds that further damage this tissue through oxidation reactions, and also a decrease in the degradation time of the patch from 45 to 30 days. Regarding this last property, Tiago Carvalho explains that "it is important that an implanted material degrades progressively, so that new cells can grow and multiply in that location, giving rise to a new tissue [a phenomenon called Bioresorbability]."
First steps toward regeneration
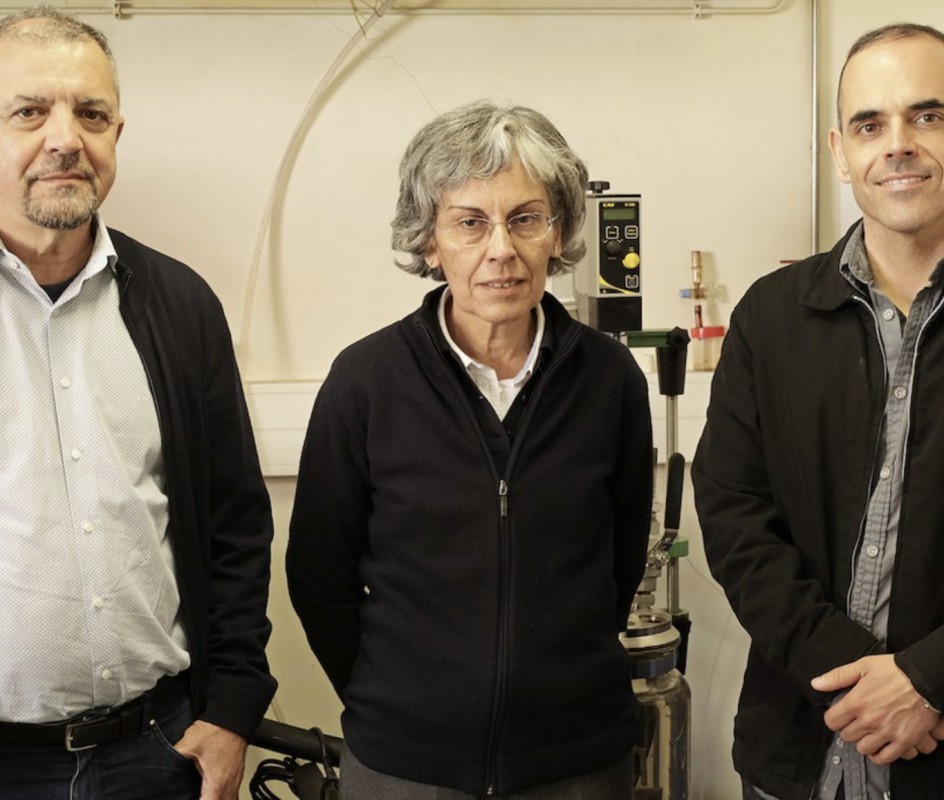
"These improvements were achieved without affecting the initial morphology, the thermal stability, the biocompatibility and the ability of the patches to incorporate and release a drug," congratulates Tiago Carvalho who, along with researchers Carla Vilela and Carmen Freire (supervisor of Tiago Carvalho), researchers at CICECO and the Department of Chemistry at UA, signed the study that also included the participation of scientists from the University of Helsinki, including Helder Santos, co-supervisor of Tiago Carvalho.
This work represents a first step towards helping the recovery of those who have suffered a myocardial infarction and who currently have as their only solutions palliative therapies or heart transplantation, an operation always surrounded by risk, but which is, in fact, the only effective form of treatment available today.
As part of this study, some in vitro biological tests have been carried out in Helsinki with these biopolymeric plasters. "The next step will be to complement these results with in vivo tests using animal models. So there are still a few more years of research before such a biomaterial can be implanted in humans," predicts the CICECO doctoral student.
This research is part of Tiago Carvalho's doctoral project focused on the use of protein fibers to develop materials to regenerate the myocardium. The project is funded by the Foundation for Science and Technology.
Related Articles
We use cookies for marketing activities and to offer you a better experience. By clicking “Accept Cookies” you agree with our cookie policy. Read about how we use cookies by clicking "Privacy and Cookie Policy".